2021 Volume No 42 – pages 264-280
Title: Evidence for osteocyte-mediated bone-matrix degradation associated with periprosthetic joint infection (PJI) |
Authors: RT Ormsby, AR Zelmer, D Yang, NJ Gunn, Y Starczak, SP Kidd, R Nelson, LB Solomon, GJ Atkins |
Address: Centre For Orthopaedic and Trauma Research, Faculty of Health and Medical Sciences, The University of Adelaide, North Terrace, Adelaide, SA, Australia, 5005 |
E-mail: gerald.atkins at adelaide.edu.au |
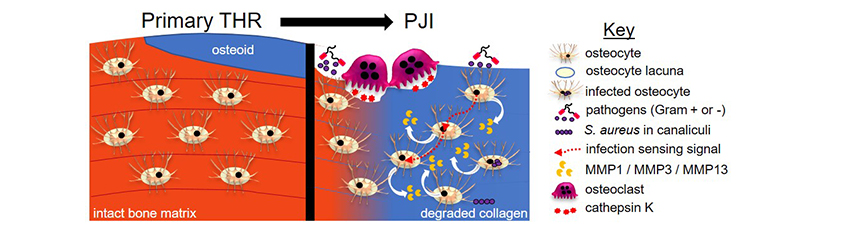
Abstract: Osteomyelitis associated with periprosthetic joint infection (PJI) signals a chronic infection and the need for revision surgery. An osteomyelitic bone exhibits distinct morphological features, including evidence for osteolysis and an accelerated bone remodelling into poorly organised, poor-quality bone. In addition to immune cells, various bone cell-types have been implicated in the pathology. The present study sought to determine the types of bone-cell activities in human PJI bones. Acetabular biopsies from peri-implant bone from patients undergoing revision total hip replacement (THR) for chronic PJI (with several identified pathogens) as well as control bone from the same patients and from patients undergoing primary THR were analysed. Histological analysis confirmed that PJI bone presented increased osteoclastic activity compared to control bone. Analysis of osteocyte parameters showed no differences in osteocyte lacunar area between the acetabular bone taken from PJI patients or primary THR controls. Analysis of bone matrix composition using Masson’s trichrome staining and second-harmonic generation microscopy revealed widespread lack of mature collagen, commonly surrounding osteocytes, in PJI bone. Increased expression of known collagenases, such as matrix metallopeptidase (MMP) 13, MMP1 and cathepsin K (CTSK), was measured in infected bone compared to non-infected bone. Human bone and cultured osteocyte-like cells experimentally exposed to Staphylococcus aureus exhibited strongly upregulated expression of MMP1, MMP3 and MMP13 compared to non-exposed controls. In conclusion, the study identified previously unrecognised bone-matrix changes in PJI caused by multiple organisms deriving from osteocytes. Histological examination of bone collagen composition may provide a useful adjunct diagnostic measure of PJI. |
Key Words: Periprosthetic joint infection, osteomyelitis, osteocyte, osteoclast, osteocytic osteolysis, perilacunar remodelling, collagen, matrix metallopeptidase. |
Publication date: October 8th 2021 |
Article download: Pages 264-280 (PDF file) |